Blog
Pregnancy: It can be a pain in the a#$
20 September 2013Pain during pregnancy - the pelvis Whilst the agony of pregnancy should only be about choosing a name and assembling the Ikea cot, for almost half of pregnant women there is the added burden of disabling pelvic pain which typically presents through the second trimester. Pregnancy related pelvic pain is a familiar issue to Physiotherapists and can be difficult to treat. This is due to the complex nature of the problem, the close proximity of the pelvis to the hip joints and low back. Also, because the pregnant body continually changes - posture, fluid and hormone levels progress, the problem you were dealing with one week is completely different to the next. The majority of pelvic pain during pregnancy occurs around the buttocks and the pubic symphysis (where the pelvis meets at the front). Typically, the onset of pain occurs around the 18th week and reaches peak intensity between the 24th and 36th week of pregnancy. This pain can radiate to other parts of the pelvis and to the upper and lower legs but can have a similar referral pattern to herniated discs, facet joint syndrome and spinal stenosis which complicates diagnosis. It is aggravated by transferring load to a single leg, such as walking, stair climbing or getting in and out of a car. Where does the problem occur? The sacroiliac joint (SIJ) is a primary source of dysfunction effected by a complex system of structures, which attempt to stabilise and control movement at the pelvis. The events which prepare the pelvis for delivery (namely the release of a hormone called Relaxin), also affect the function of the pelvis to transfer load (whilst walking) and compromise stability. This can lead to disabling pain and impaired function during pregnancy which requires astute assessment, differential diagnosis and applied intervention by a Physiotherapist.
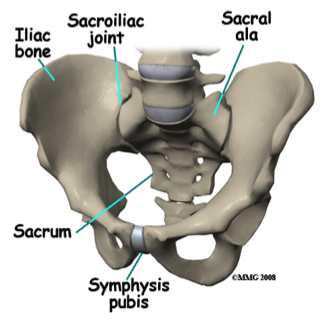 The sacrum sits between two large pelvic bones called ilia. The attachment of the sacrum to the ilia is the sacroiliac joint. The joint surfaces are flat (to allow forward bending) and are therefore vulnerable to shearing forces. Normally held strongly together by a system of ligaments and muscles acting over the joint, when pregnant the ligaments and muscles are unable to sufficiently support the pelvis and it is the asymmetric shearing of the joint that causes pain. The laxity of ligaments, ineffective timing and activation of surrounding muscles occurs during pregnancy for various reasons:
1. Relaxin is a hormone which peaks at the 12th gestational week, with a gradual reduction until the 17th week. Relaxin decreases the intrinsic strength of connective tissue to allow it to stretch (prepares the pelvis to enable it to separate when giving birth).
2. Due to pregnancy related changes in posture, the deep (core) muscle system which controls the stability of the pelvis is stretched and is unable to work at the optimum tension. The global (bigger muscles designed to move rather than stabilise) muscle system is also affected with the splitting (diastasis) of the abdominals.
3. Increased ligament laxity also allows separation of the pubic symphysis in preparation for birth. A 10mm diastasis of the pubic symphysis is not uncommon in pregnancy.
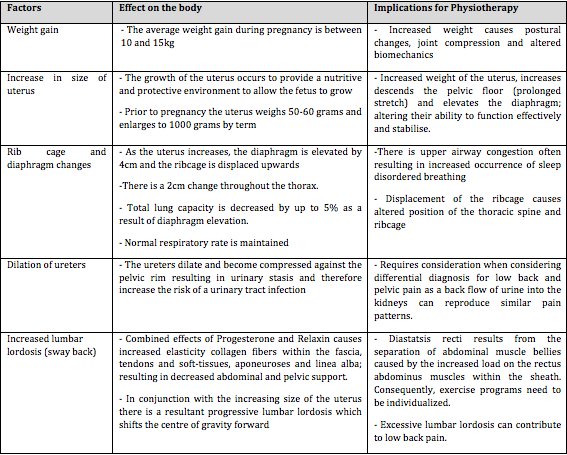
The effect of pregnancy on the body
The sacrum sits between two large pelvic bones called ilia. The attachment of the sacrum to the ilia is the sacroiliac joint. The joint surfaces are flat (to allow forward bending) and are therefore vulnerable to shearing forces. Normally held strongly together by a system of ligaments and muscles acting over the joint, when pregnant the ligaments and muscles are unable to sufficiently support the pelvis and it is the asymmetric shearing of the joint that causes pain. The laxity of ligaments, ineffective timing and activation of surrounding muscles occurs during pregnancy for various reasons:
1. Relaxin is a hormone which peaks at the 12th gestational week, with a gradual reduction until the 17th week. Relaxin decreases the intrinsic strength of connective tissue to allow it to stretch (prepares the pelvis to enable it to separate when giving birth).
2. Due to pregnancy related changes in posture, the deep (core) muscle system which controls the stability of the pelvis is stretched and is unable to work at the optimum tension. The global (bigger muscles designed to move rather than stabilise) muscle system is also affected with the splitting (diastasis) of the abdominals.
3. Increased ligament laxity also allows separation of the pubic symphysis in preparation for birth. A 10mm diastasis of the pubic symphysis is not uncommon in pregnancy.
The effect of pregnancy on the body

 Getting the right diagnosis!
The pelvis is a complex area and pain can be often confused with low back or hip pain. Therefore a good Physiotherapist will develop a diagnosis by clinically assessing the lumbar spine, hip and pelvis to differentiate between the areas and localise a source of pain. This is important as the path of treatment will change based on the diagnosis.
Magnetic resonance imaging (MRI), computed tomography (CT) and bone scans of the SIJ cannot reliably determine whether the joint is the source of pain. The use of ultrasound diagnostically can determine the effectiveness of the stabilising muscles.
Treating pregnancy related pelvic pain
The modalities listed here are those which have been shown to be most appropriate and helpful.
1. Supervised exercise: There is no doubt in the literature that a supervised exercise program is the best form of Physiotherapy for this issue (either on land or in the pool). Treatment should begin with the retraining of the local muscle system (core muscles including pelvic floor); Because there is room to make the pain worse with the wrong exercises or by performing the right exercises incorrectly, any prescribed program should be supervised initially and individualised.
2. Mobilisation/ Manual treatment including massage: Mobilisation techniques and soft-tissue release are appropriate for treatment. It must be recognised that ligaments of the pelvis remain stretched for as long as 6-12 months following delivery and joints are more mobile as a result. This should therefore be considered before undergoing aggressive manual therapy techniques such as manipulation of the pelvic joints.
3. The pelvic belt: The prescription of a pelvic belt is common practice as it has been shown to produce relief. The basis for the use of the pelvic belt is that the joint surfaces are placed in a position of maximum stability. The pelvic belt - whilst not the next thing to hit the fashion runways, allows decreased pain following activity and increases tolerance for daily activities.
4. Education: Understanding the issue and how to retrain muscles, alleviate pain and to avoid aggravating factors is a helpful adjunct to treatment.
5. Hydrotherapy: Hydrotherapy has been shown to be effective for reducing pain and improving movement in women with pelvic pain. The benefit of water exercise is it is low impact, the whole body can be exercised with the training of core and global muscles systems, integrated.
6. Acupuncture: Whist acupuncture alone has not been shown in the scientific literature to be helpful in reducing pregnancy related pelvic pain, one quality study found acupuncture and stabilising exercises decreased pain greater than stabilising exercises alone (Elden et al. 2005).
It is always best to prevent pelvic instability and exercise programs can start prior to pregnancy. However, if pain develops during pregnancy, outcomes are better if treated it in the initial stages.
Getting the right diagnosis!
The pelvis is a complex area and pain can be often confused with low back or hip pain. Therefore a good Physiotherapist will develop a diagnosis by clinically assessing the lumbar spine, hip and pelvis to differentiate between the areas and localise a source of pain. This is important as the path of treatment will change based on the diagnosis.
Magnetic resonance imaging (MRI), computed tomography (CT) and bone scans of the SIJ cannot reliably determine whether the joint is the source of pain. The use of ultrasound diagnostically can determine the effectiveness of the stabilising muscles.
Treating pregnancy related pelvic pain
The modalities listed here are those which have been shown to be most appropriate and helpful.
1. Supervised exercise: There is no doubt in the literature that a supervised exercise program is the best form of Physiotherapy for this issue (either on land or in the pool). Treatment should begin with the retraining of the local muscle system (core muscles including pelvic floor); Because there is room to make the pain worse with the wrong exercises or by performing the right exercises incorrectly, any prescribed program should be supervised initially and individualised.
2. Mobilisation/ Manual treatment including massage: Mobilisation techniques and soft-tissue release are appropriate for treatment. It must be recognised that ligaments of the pelvis remain stretched for as long as 6-12 months following delivery and joints are more mobile as a result. This should therefore be considered before undergoing aggressive manual therapy techniques such as manipulation of the pelvic joints.
3. The pelvic belt: The prescription of a pelvic belt is common practice as it has been shown to produce relief. The basis for the use of the pelvic belt is that the joint surfaces are placed in a position of maximum stability. The pelvic belt - whilst not the next thing to hit the fashion runways, allows decreased pain following activity and increases tolerance for daily activities.
4. Education: Understanding the issue and how to retrain muscles, alleviate pain and to avoid aggravating factors is a helpful adjunct to treatment.
5. Hydrotherapy: Hydrotherapy has been shown to be effective for reducing pain and improving movement in women with pelvic pain. The benefit of water exercise is it is low impact, the whole body can be exercised with the training of core and global muscles systems, integrated.
6. Acupuncture: Whist acupuncture alone has not been shown in the scientific literature to be helpful in reducing pregnancy related pelvic pain, one quality study found acupuncture and stabilising exercises decreased pain greater than stabilising exercises alone (Elden et al. 2005).
It is always best to prevent pelvic instability and exercise programs can start prior to pregnancy. However, if pain develops during pregnancy, outcomes are better if treated it in the initial stages.